Sylvester Brings Leading-Edge Multidisciplinary Care to Brain Tumor Patients

Advanced diagnostic technology, innovative surgical procedures and a wide range of clinical trials are just a few of the reasons patients with malignant and benign brain tumors seek care from the experienced multidisciplinary team at the Sylvester Comprehensive Cancer Center Brain Tumor Initiative (BTI), part of the University of Miami Health System and the Miller School of Medicine.
“As the only National Cancer Institute (NCI)-designated cancer center in South Florida, Sylvester brings together specialists in many disciplines,” said Ricardo J. Komotar, M.D., a top neurosurgeon in Florida, and director of the BTI – one of two collaborative programs that deliver leading-edge patient care. “Our extensive experience allows us to make the most accurate diagnoses, generate the most effective treatment plans, and conduct brain tumor research studies that ultimately lead to the best outcomes for adult and pediatric patients.”
World-Class Clinical Teams
Sylvester’s Brain Tumor Initiative offers patients the advantages of a world-class clinical team with expertise from more than 30 specialties throughout the University of Miami Health System. The team includes internationally recognized neurosurgeons, as well as neuropathologists, radiation oncologists and neuro-oncologists who share their knowledge to deliver personalized care to each individual. Brain tumor patients gain access to clinical trials, new, cutting-edge medical and radiation treatments, and minimally invasive surgical techniques that enhance outcomes.
Complementing the Brain Tumor Initiative is the UM Skull Base Surgery Program, founded in 1995, which focuses on tumors affecting the entire region of the head and neck, and specifically the brain, the orbits and the skull base, including the nasal cavity and sinuses.
“Our brain tumor and skull base surgery programs are the crown jewels in our multidisciplinary specialty practice at the Miller School,” said Allan D. Levi, M.D., Ph.D., professor and chair of neurosurgery, chief of neurosurgery at Jackson Memorial Hospital, and the Robert M. Buck Distinguished Chair in Neurological Surgery
Led by renowned neurosurgeon Jacques Morcos, M.D., professor and co-chairman of the Department of Neurosurgery, the Skull Base Surgery Program is a national and international referral resource for patients with tumors, such as meningiomas, pituitary adenomas, acoustic neuromas, chordomas, cancers of the sinuses, among many others. Since 2006, the program has embraced minimally invasive surgery, including endonasal endoscopic approaches, which has expanded dramatically in breadth and depth over the years.
An international leader in the surgery of complex tumors of the brain, base of the skull as well as the surgery of complex vascular lesions, Dr. Morcos is a former president of the North American Skull Base Society, as well as the Society of University Neurosurgeons, and now serves on the board of the American Association of Neurological Surgeons. “Through the synergy of our dedicated practitioners, including our talented colleagues in the Department of Otolaryngology, the skull base team has achieved many breakthroughs, the latest being implanting the first auditory brainstem implant (ABI) in an acoustic neuroma patient in Florida,” said Dr. Morcos.
Diagnosing the tumor
For all types of brain and skull base tumors, UM’s board-certified neuropathologists use state-of-the-art tools to determine the most effective treatment. “Testing tissue samples helps refine the diagnosis, and identify direct molecular targets for highly effective drug therapy,” said Sakir Humayun Gultekin, M.D., director of clinical and molecular neuropathology for the BTI. “They also help in predicting outcomes for individual patients.”
Those findings are evaluated by a diverse team of Miller School specialists in fields such as neurology, endocrinology, ophthalmology, oculoplastic surgery, head and neck surgery, rhinology, neuro-otology, otolaryngology, and radiation oncology. All these specialists meet weekly as a group and collaborate to determine the best treatment approach. “The whole is simply larger than the sum of its parts,” said Dr. Morcos.
Research
Clinical research of treatments, radiation and surgical approaches provides a solid foundation for quality patient care. “We usually have 10 to 15 clinical trials underway at any one time,” said Macarena de la Fuente, M.D., assistant professor of neurology and interim chief of the Neuro-oncology Division. “Because our program has a large volume of patients, we are able to conduct more trials exploring different types of therapies for brain tumors.”
Michael E. Ivan, M.D., director of research at the BTI, president-elect of the Florida Neurosurgical Society, and co-leader of the Sylvester neuro-oncology site disease group, leads the translational research program as well as its tumor bank, which has more than 2,000 specimens, making it one of the largest in the nation. “By investigating our patients’ tumors in our lab, we can then quickly develop new technologies that we can bring back to the patient’s bedside,” he said. “There are still many unknowns, but we are making new discoveries every day in the lab.”
Eric Albert Mellon, M.D., Ph.D., assistant professor of radiation oncology and co-leader of Sylvester’s neuro-oncology site disease group, is leading a new clinical trial for brain metastases. “All of our specialists publish articles regularly on brain tumors, present at international conferences, and collaborate on treatment guideline development,” he said.
Education
A major teaching center for neurosurgeons, the Miller School has one of the nation’s largest teams for brain tumor treatment, and its neurosurgeons have unparalleled experience with the highest volume of cases in Florida. The Department of Neurosurgery recently opened a world-class training facility, the C.A.N.E.S. lab, in a joint effort with the Department of Otolaryngology for research and education in skull base and microsurgery. “This facility attracts specialists from all over the world who come to learn from the expertise of UM specialists from both departments,” said Dr. Morcos.
Leadership in tumor procedures
Sylvester’s neurosurgeons use the latest imaging and minimally invasive treatment technology to remove tumors safely, while shortening hospital stays and accelerating recoveries. For instance, Dr. Ivan recently led the team by introducing two new surgical technologies at UM, which allow surgeons to make more accurate decisions during surgery. The first, 5-ALA (5-aminolevulinic acid) fluorescence, helps surgeons visualize malignant tissue during surgery, while the second, the NIO Imaging System, drastically decreases the time of procedures by rapidly processing and evaluating the tumor tissue.
The BTI’s neurosurgeons have deep experience with leading-edge procedures, such as awake-brain mapping for the treatment of gliomas, endonasal surgery and laser interstitial thermal therapy. Dr. Komotar – whose training includes neuropharmacology as well as specialized brain neurosurgery – performed the state’s first robotic-assisted brain biopsy in January 2019, using the ROSA robot to guide a needle biopsy for diagnosing a patient’s tumor – a minimally invasive technique.
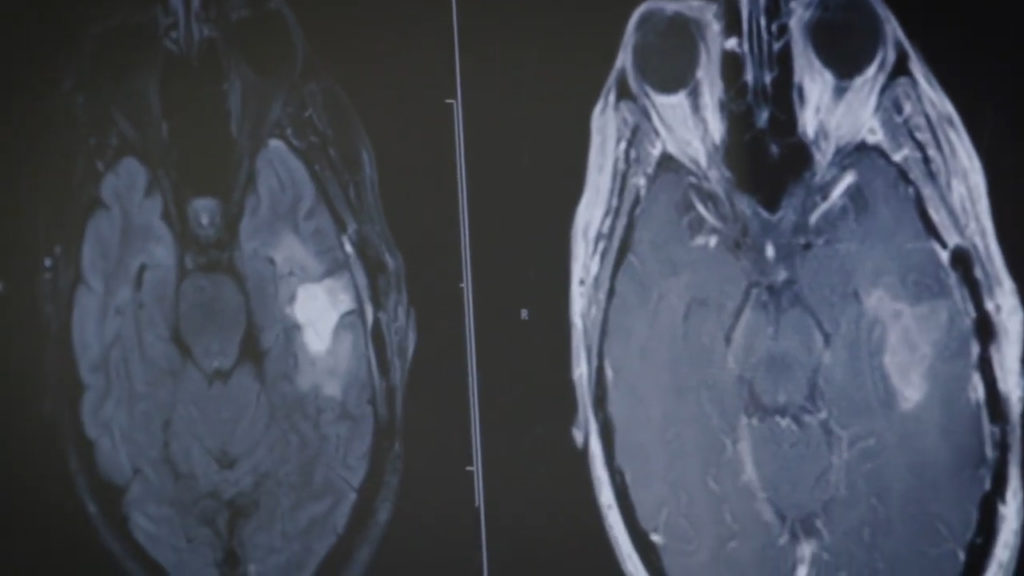
Many brain tumor patients receive neuroradiation treatments in conjunction with surgery to destroy malignant cells. Dr. Mellon and Tejan Diwanji, M.D., assistant professor of radiation oncology, are skilled in using magnetic resonance imaging (MRI) for brain and spine tumors, and use advanced technology like the GammaKnife, ViewRay, and HyperArc to help diagnose and treat the varied types of benign and malignant tumors.
The Miller School Department of Neurosurgery’s Gamma Knife radiosurgery center is directed by Howard Landy, M.D., and Ronald J. Benveniste, M.D., Ph.D., also specializes in brain tumor surgery and radiosurgery. Carolina Benjamin, M.D., a graduate from New York University, recently joined the neurosurgery team to serve the expanding cranial practice.
As for nonsurgical care, Dr. de la Fuente brings extensive experience in medical treatments for brain tumors, including therapies to strengthen the immune system. With neuro-oncologist Deborah Heros, M.D., and Maria del Pilar Guillermo Prieto Eibl, M.D., Dr. de la Fuente leads collaborative, multicenter, national and international trials for primary brain tumors.
A coordinated approach to patient care
Sylvester’s coordinated approach to patient care makes a positive difference in patient outcomes. Eric Tate traveled more than 300 miles to be treated by the Brain Tumor Initiative. “I had neurosurgery for a glioblastoma in June and will have more radiation and chemotherapy as well,” said Tate. “It’s been an ordeal, but I’m very happy with the care I’ve received.”
A rare but deadly form of cancer, glioblastoma is most common in older patients, but can occur at almost any age, said Dr. de la Fuente. “The symptoms may include severe headaches, seizures or changes in vision, sensation, balance or cognitive thinking, depending on where the tumor is located in the brain.”
Tate, a 30-year-old medical sales representative in rural Hernando County, said he began experiencing headaches, fatigue and vision problems in 2017. After diagnostic scans revealed the brain tumor near the optic nerve to his left eye, he had emergency surgery at a Tampa hospital, followed by 17 months of chemotherapy and radiation. However, the glioblastoma returned, and his girlfriend, Gina deAngelo, started looking at clinical trials and chose the Sylvester’s BTI for treatment.
When Tate turned to the brain tumor program, he opted for aggressive standard care as well as enrolling in a clinical trial. “It looks like Dr. Komotar’s surgery was successful,” he said. “My vision is back to normal, and I am cautiously optimistic about the future.”
Written by Richard Westlund for Inventum.
Tags: Brain Tumor Initiative, Dr. Ricardo Komotar, Gamma Knife radiosurgery center, Sylvester Comprehensive Cancer Center
