Experts: The Efficacy of a Colonoscopy
A provocative study by Bretthauer et al. in the New England Journal of Medicine (NEJM) was published on October 9, 2022. The study (the NordICC trial) was a randomized control trial from centers in Poland, Norway, Sweden, and the Netherlands.
How the study worked:
Men and women in the four countries who were 55 to 64 years of age and had not previously undergone screening were identified through population registries and randomized into two groups:
- “Invited” colonoscopies (received invitations to undergo a single screening colonoscopy)
- “Usual care” (no invitation)
The participants were followed for a median duration of 10 years. The primary outcome was the development of colorectal cancer (CRC) or death from CRC.
Among 84,585 participants (28,220 in the invited group and 56,365 in the usual care group), the risk of CRC at 10 years was 0.98% (259 cases) in the invited group and 1.20% (622 cases) in the usual-care group, for a risk ratio of 0.82 (95% confidence interval [CI], 0.70 to 0.93).
The risk of CRC–related death at 10 years was 0.28% (72 deaths) among participants in the invited group and 0.31% (157 deaths) among those in the usual-care group (risk ratio, 0.90; 95% CI, 0.64 to 1.16).
In essence, the authors of the study found that CRC incidence was reduced by 18% in the “invited” group, but that there was no significant mortality reduction at 10 years.
An adjusted per-protocol analysis was done and showed benefit in both incidence and mortality (risk ratio 0.50 (95% CI, 0.27 to 0.77)) if all participants who were assigned to screening had undergone screening. That is half the risk of CRC-related death.
These findings have led to a great deal of press and concerns about the efficacy of colonoscopy.
However, a close reading of the study is imperative. We highlight several issues here that have been also been addressed by national societies, including the American College of Gastroenterology and the American Society of Gastrointestinal Endoscopy.
Indeed, the editorial accompanying the NEJM article also cautioned against misinterpreting the study’s findings.
1. Only 42% of the invited group underwent colonoscopies.
The intervention was not colonoscopy itself, but a one-time invitation by the trial authors to receive a colonoscopy. While it is fair to say that this one-time invitation did not reduce CRC-related death, it must also be pointed out that those who underwent colonoscopy had only half the risk of CRC-related death.
In other words, the invitation may not have been effective, but the colonoscopies were.
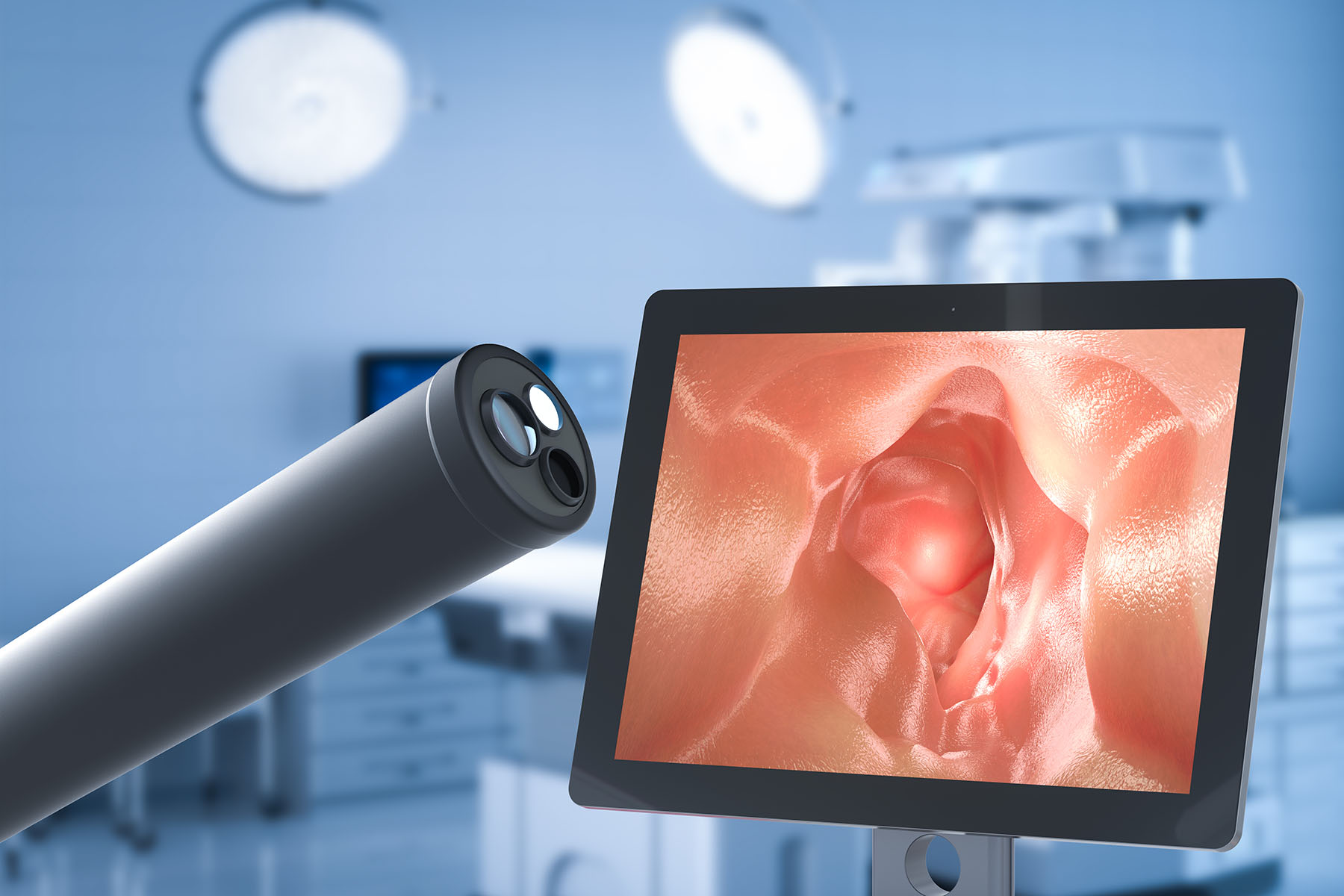
2. Adenoma detection rate, or ADR, is how we grade ourselves as gastroenterologists.
If we are not detecting enough adenomatous polyps (the types of polyps that turn into cancer), this suggests we are performing low-quality endoscopies and missing (not seeing or detecting) colon cancers. In the U.S., we have a minimum benchmark of 25% ADR.
The endoscopists performing the colonoscopies in the NordICC study had much lower ADRs — as low as 14%, in one country. In total, based on the author’s prior publications, a third of the colonoscopies performed in the U.S. do not meet our benchmark for quality, indicating the potential for missed cancers.
All of this underscores the need for high-quality colonoscopies to prevent CRC risk and CRC-related death.
3. The 10-year follow-up time of the study was relatively short.
The process by which normal colon cells turn cancerous is lengthy and can take in excess of 10 years. Moreover, the age range of NordICC study participants did not extend past 64 years. Including older individuals who were eligible for screening may have led to more pronounced findings. So even with this study, we may see different or more exaggerated findings when the authors conduct their next analysis, which they plan to do in five years.
Other considerations include whether these countries (Scandinavian and Eastern European) have different CRC rates than the U.S. In this country, it is well known that racial minorities, particularly African Americans, are more likely to develop and to die from CRC. In addition, the authors did not comment on the location of the cancers — an area of intense interest in the U.S. as we are seeing “proximal” and “distal” cancers behave differently.
Despite these issues, we believe this study is important, in part because it highlights one of the more difficult aspects of CRC prevention: convincing eligible people to undergo screening colonoscopies.
A prior study has demonstrated that invitations do improve compliance, but there is clearly more work to be done. Community outreach and education efforts like those at Sylvester Comprehensive Cancer Center at the University of Miami Health System include self-assessment tools, and focus on raising awareness of risk factors and the value of regular colonoscopies.
Researchers are also developing ways to enhance gastroenterologists’ colonoscopy skills so that patients get the best possible examination and polyps are removed before they turn into cancer.
Overall, however, we are concerned about the headlines and messaging that have arisen from misinterpretation of the NordICC study.
- CRC is currently the second leading cause of cancer deaths in the U.S.
- The lifetime risk of getting CRC is approximately 4%
- Early-onset CRC is on the rise
Colonoscopy is one of a few guidelines and society recommended modalities to decrease that risk.
We strongly encourage our patients to continue with their recommended screenings, and we look forward to future research that will help us continue to prevent CRC and CRC-related deaths.
Written by
Tags: colon cancer or rectal cancer, Dr. Daniel Sussman, Dr. Shria Kumar, early stage, risk of colorectal cancer, risk of developing colorectal, screening tests, testing colonoscopy