Significant Advances in Identifying and Treating Tay-Sachs Disease
Tay-Sachs disease is a neurodegenerative disorder that typically leads to death in children by the age of 5. There is no cure. Existing therapies only manage the symptoms or, in the best cases, slow progression.
For parents, a diagnosis can be like receiving a death sentence for their child, says Deborah Barbouth, M.D., a clinical geneticist for the University of Miami Health System. However, “there are many promising therapies being investigated,” she adds, and technology is advancing at such a rate that this inherited condition may one day be wiped out in most communities.
The cause of Tay-Sachs Disease
Tay-Sachs is caused by a defect in a gene (HEXA) on chromosome 15. This altered gene leads to a deficiency of the enzyme beta-hexosaminidase A. This enzyme is needed to break down a fatty substance called GM2 ganglioside. If this fatty substance isn’t eliminated, it accumulates in the brain and spinal cord, which, in turn, damages nerve cells and causes neurological problems.
Symptoms usually develop when a baby is about 3 to 6 months old. These can include seizures, muscle stiffness, difficulty swallowing, loss of vision or hearing and being slow to reach developmental milestones. Tay-Sachs affects about one in 360,000 babies born in the general population, which is about 10 new cases per year nationwide. However, in some populations — Ashkenazi Jews, French Canadians and Cajuns in Louisiana — the prevalence is much higher. That means that more people within those populations are carriers of an altered gene HEXA. A carrier does not exhibit any symptoms because you need two copies of the altered gene for the disorder to manifest itself.
Tay-Sachs is autosomal recessive. What does that mean?
A child develops it only when both parents are carriers of the defective gene. Even then, there’s only a 25% chance the child will inherit the disease. However, the child will have a 50% chance of being a carrier. In the general U.S. population, the carrier rate is around one in 250. But among Ashkenazi Jews, one in 27 is a carrier. French Canadians and Louisiana’s Cajun community have a similar carrier rate as eastern European Jews.
The advent of genetic screening, however, has meant that the number of diagnosed cases has declined significantly — by 90% for Jews, in one estimate. In fact, before widespread screening began, about 50 to 60 Jewish children were born with Tay-Sachs each year in the U.S. and Canada. It is estimated that this number has fallen to just two to five cases per year. Screening programs in other high-risk populations have not been as widespread, which means that the decline in Tay-Sachs births hasn’t been as dramatic.
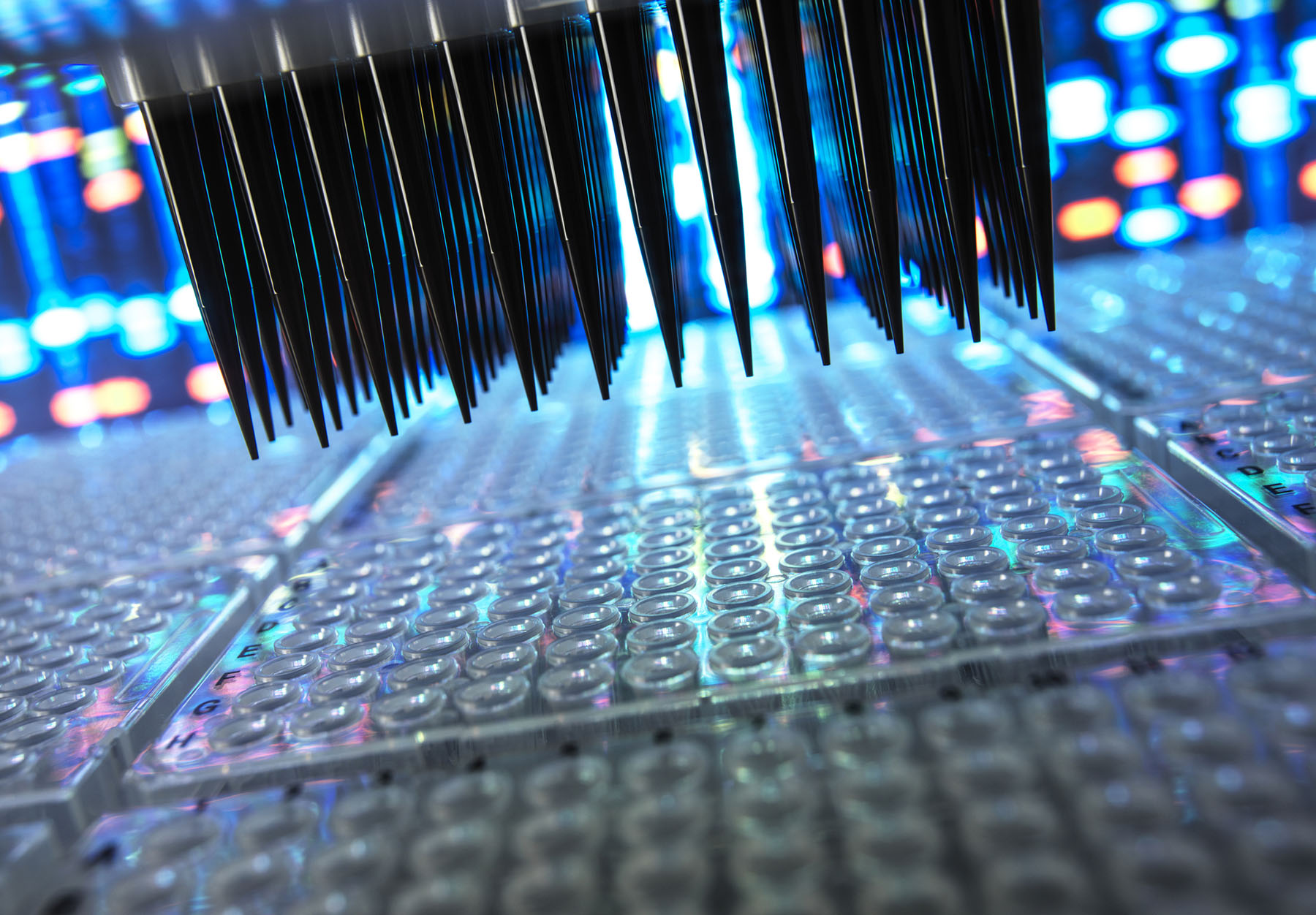
Genetic screening, Dr. Barbouth says, has progressed so much that it can identify mutations in the HEXA gene with “high precision.” Such screening has also become more affordable, which makes it easily accessible to a wider range of people. Guidelines recommend universal or expanded screening for everyone, regardless of ethnicity. Plus, most are mail-in home kits that use saliva or cheek swabs. These home kits can test for many other genetic disorders, including cystic fibrosis, sickle cell anemia and fragile X syndrome, among more than 700 other conditions.
Other recent breakthroughs in the study of Tay-Sachs involve:
Gene therapy.
Researchers in Boston were able to insert copies of the HEXA gene into brain cells of two children with Tay-Sachs. That allowed the children to produce the missing enzyme critical to breaking down the fatty substances that clog the brain and eventually damages nerve cells. Also, other gene editing methods have been shown to be effective in animals. This development has been met with cautious optimism. The Cure Tay-Sachs Foundation calls gene therapy “one of the most significant advancements in recent years.”
Dr. Barbouth says, “Gene therapy, or a variation, is coming for (Tay-Sachs). It’s just a matter of time.” She is hoping that, as gene therapy technology advances, “we can one day treat (the condition) in utero.”
Enzyme replacement therapy.
Researchers are figuring out ways to deliver synthetic hexosaminidase A enzymes directly to the brain by using special delivery systems. In addition, they are exploring fusion proteins and enzyme modifications to improve stability and uptake by brain cells. This is in the very early stages.
Newer and more refined approaches in physical, occupational and related therapies.
While these therapies are not in clinical trials nor do they slow or stop the disease, they provide comfort to patients. These include:
- Tech-enabled communication aids (symbol boards or voice-output devices)
- Better chest physiotherapy (targeted vibrating vests or suction devices) that clears mucus and prevent infections
- Assistive technology (eye-tracking devices or adaptive switches) to help patients interact with their environments
- Adaptive positioning systems (custom seating and braces) to improve posture and reduce pressure sores
- Neuromuscular stimulation to delay joint contractures and reduce pain.
Written by Ana Veciana-Suarez for UHealth.
Tags: Dr. Deborah Barbouth, gene therapy, genetics, research studies, tay-sachs disease

