How is HPV Connected to Cancer?
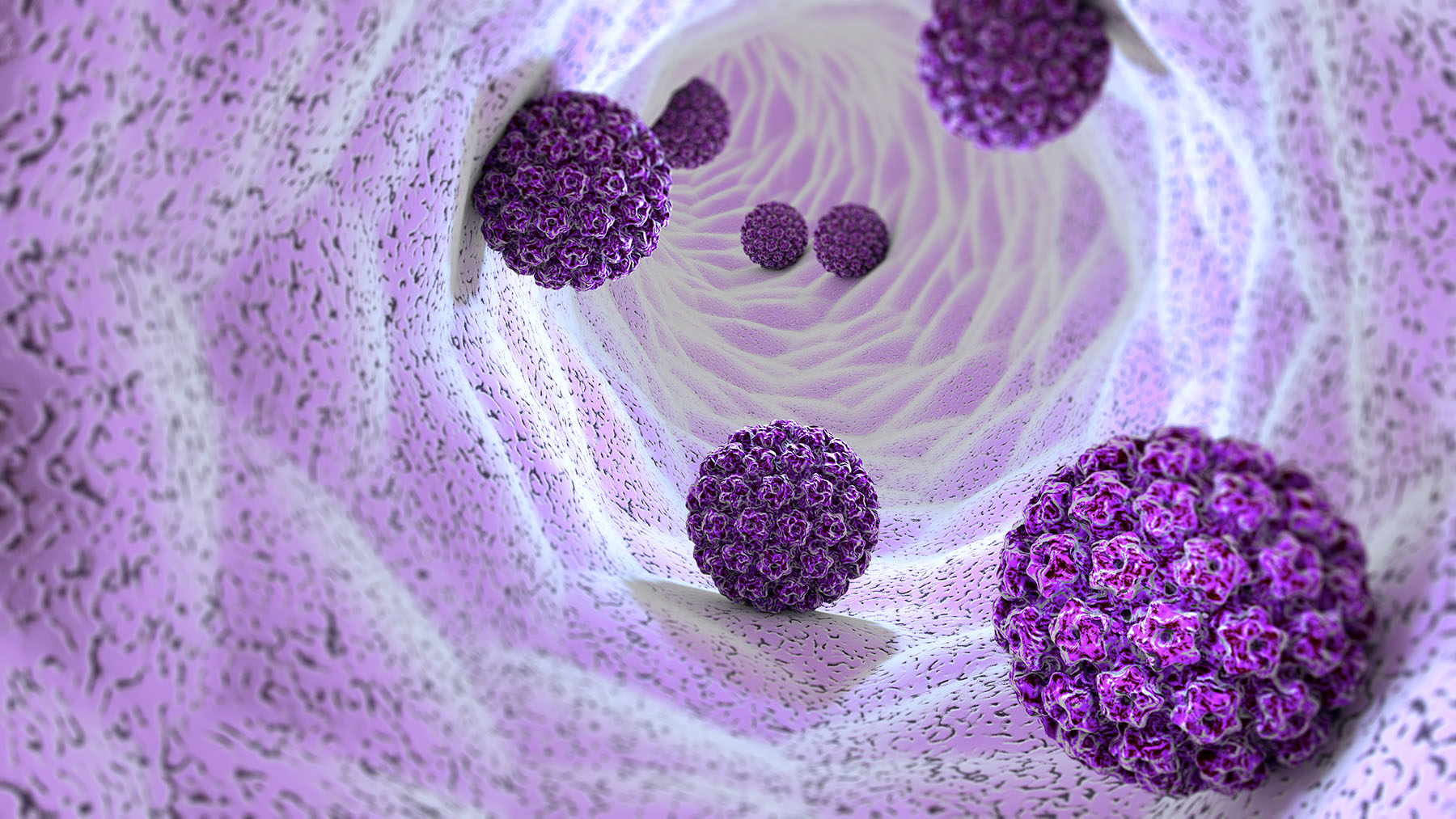
An estimated 79 million Americans are currently infected with human papillomavirus (HPV).
Most people with HPV don’t experience any symptoms. For many, the virus goes dormant, becomes undetectable, or clears up entirely on its own.
For others, HPV infection can develop into warts and/or cancer.
There is currently no available cure for HPV infection.
How is HPV connected to cancer?
HPV infection can develop into cancers of the cervix, vulva (outer part of female genitals), vagina, penis, anus, and throat (base of the tongue and tonsils). There are approximately 200 HPV strains. Some are low risk, while other strains can trigger inflammation that, over time, causes cancer in both men and women.
Nearly all cases of cervical cancer and most vaginal cancers are tied to HPV infection.
“In someone with a competent/functional immune system, the time from infection to cancer can be up to 10 years,” says Matthew Schlumbrecht, M.D., a gynecologic oncologist with Sylvester Comprehensive Cancer Center. “In women who are immunocompromised (HIV disease, or on immunosuppressive medications), this time can be much shorter.”
The number of men and women diagnosed with anal cancer each year is on the rise, and more than 90% of these cases are caused by HPV.
HPV DNA may be detected in over 20% of penile tumor cells, and “50 to 60% of penile cancers are associated with HPV infection,” says Chad Ryan Ritch M.D., a urologic oncologist with Sylvester. “It may take many years before HPV infection manifests as cancer, and fortunately, most HPV infections in men do not progress to penile cancer.”
Signs of HPV infection are found in more than two out of three oropharyngeal cancers, which include cancers of the back of the throat, base of the tongue, and tonsils.
“It appears that persistent HPV infection is an important risk factor,” says Elizabeth Franzmann, M.D., a head and neck surgeon with UHealth. “While cancer can occur as few as five years [after HPV infection], the virus is generally thought to have a latency of over 10 years.”
Protect yourself, your partners, and your child from HPV infection
Get the HPV vaccine.
The HPV vaccine (Gardasil in the U.S.) can protect you against 80% of HPV-caused cervical cancers and five other types of cancer. It also prevents 90% of genital warts caused by HPV.
Because both men and women can spread HPV to their sexual partners, it’s equally important for boys and girls to get vaccinated against HPV to protect themselves and their future partners.
The HPV vaccine should not be seen as a sexually transmitted infection vaccine. It is a cancer prevention vaccine.
Dr. Schlumbrecht
“In unvaccinated women, the risk of becoming infected with HPV is approximately 80%.”
Why do children need to be vaccinated?
To be most effective, the HPV vaccine must be administered before any possible exposure to the virus.
HPV is transmitted from skin-to-skin contact, including genital-genital, oral-genital, or other skin-genital contacts.
“Autoinocculation (fingernails) and deep mouth kissing are probably of little importance compared to oro-genital transmission. The average time from infection to development of cancer is over 10 years,” says Dr. Franzmann.
Young people can first be exposed during intimate encounters with a partner that don’t involve penetrative sexual intercourse. While parents of adolescents might be most concerned about unplanned pregnancies, sexually transmitted infections like HPV can be transmitted before your child is “having sex.”
According to the American Cancer Society, “even if a person delays sexual activity until marriage, or only has one partner, they are still at risk of HPV infection if their partner has been exposed.”
“We recommend the vaccination of children, both boys and girls, because the virus takes many years and even decades to form into oropharyngeal cancer,” Dr. Franzmann says.
“Based on the observed link between HPV infection and cancers of the tonsils, base of the tongue, soft palate, and uvula — and the safety and efficacy shown of the currently available HPV vaccines in preventing oral HPV infection — the American Head and Neck Society, the American Academy of Otolaryngology, and the Head and Neck Cancer Alliance all strongly encourage HPV vaccination of both boys and girls for prevention of these cancers as well as anogenital cancers.”
The Gardasil vaccine should be given to girls and boys between 9 and 12 years old.
Before age 13, children should get two doses of the vaccine 6 to 12 months apart. Those who get the first shot after their 15th birthday need three doses, given over six months, to be fully covered.
Following a conversation with your doctor and testing, you may choose to get vaccinated between the ages of 27 and 45, based on your unique risk factors. HPV vaccination is not generally recommended for those older than age 26 because most people have been exposed to the virus by this age.
Talk to your doctor to learn more about your risk based on your medical history and sexual activity.
HPV screening
Ladies, when was your last pap smear?
Pap smear tests are the first line of detection for abnormal (and pre-cancerous) cells in the cervix. It’s highly recommended that you get a pap smear every three years (or every five years in combination with HPV tests). When a pap smear reveals abnormal cells, a procedure called a colposcopy or an HPV DNA test may be recommended to confirm HPV infection. In July 2020, the American Cancer Society updated its HPV testing recommendations to include getting an HPV test every five years, from ages 25 to 65.
Speak to your primary care physician or gynecologist to discuss how often you or your daughter should get a pelvic exam with cervical swab testing. Recommendations are based on your age, medical history, and sexual activity.
There is currently no screening test for HPV in men and teenage boys. When genital warts are present on the penis or groin, they may be tested for HPV. Because of this, the virus often goes undetected in males and spreads from partner to partner.
Sexual protection
Nearly all sexually active people are exposed to HPV at some point in their lifetime. The majority of those who are unvaccinated for the virus get infected. Using a condom or dental dam every time you have sex can reduce your chances of getting HPV from your partner(s), even in sexually monogamous relationships. But, all intimate skin-to-skin contact still carries some risk of spreading and catching HPV.
Treatment for HPV infection
There is no cure for HPV infection. When warts caused by the virus are present, they can be removed by a doctor or treated with medications. This can lower the chance of spreading the virus to others, but some risk of transmission remains even when warts aren’t visible.
Written by Dana Kantrowitz, a contributor to UMiami Health News. Medically reviewed again in February 2023.
Originally published on: July 11, 2022
Tags: cancer care in Miami, cancer research in Miami, HPV infection, HPV vaccine, human papillomavirus
