Risky Business: STDs Are on the Rise; Here’s Why

Once again the U.S. broke a public health record last year — but not in a good way.
Sexually transmitted diseases continue to inch upward, according to new data from the Centers for Disease Control and Prevention, and that’s coming off record-setting years in 2014, 2015 and 2016. In fact, the country has the highest STD rate of any Western industrialized country in the world, a dubious distinction that many public health officials say could be preventable.
Almost 2.3 million cases of chlamydia, gonorrhea and syphilis were diagnosed in 2017, more than the record set back in 2016. The cases are widespread, too, diagnosed in both urban and rural settings and across socioeconomic boundaries. The CDC report said previous progress in slowing the spread of these diseases, primarily syphilis, gonorrhea and chlamydia, was “sliding backward. It is evident the systems that identify, treat, and ultimately prevent STDs are strained to near-breaking point.”
In South Florida, this report comes as no surprise. “We mirror those numbers both in Florida in general and South Florida, specifically,” says Dr. Guillermo “Willy” Prado, director of Prevention Science and Community Health within the University of Miami’s Department of Public Health Sciences. “Unfortunately, it’s been a trend here and elsewhere and it’s been persistent for several years. We’re obviously in an upward cycle.”
Among the alarming findings:
- Syphilis diagnoses, both primary and secondary, zoomed 76 percent in one year, from 17,375 to 30,644 cases. About 70 percent of those cases were found in gay, bisexual and other men who have sex with men. (Primary and secondary syphilis are the most infectious stages of the disease.) However, the CDC also found increases across demographics, including heterosexual men and women. It also noted an uptick among pregnant women, which means these infections are spreading to their babies.
- Gonorrhea cases shot up 67 percent, from 333,004 to 555,608 cases. Pushing those numbers is the nearly double the rate among men, but women also showed increases in cases for a third year in a row. It was also most common in young people 15 to 24 years of age.
- Chlamydia, the most common condition reported to CDC, remained somewhat steady, with more than 1.7 million cases diagnosed in 2017. Of those, 45 percent were reported among 15- to 24-year-old females — a troubling statistic because the disease can leave a woman infertile by scarring her reproductive organs.
Cases also on the rise in South Florida
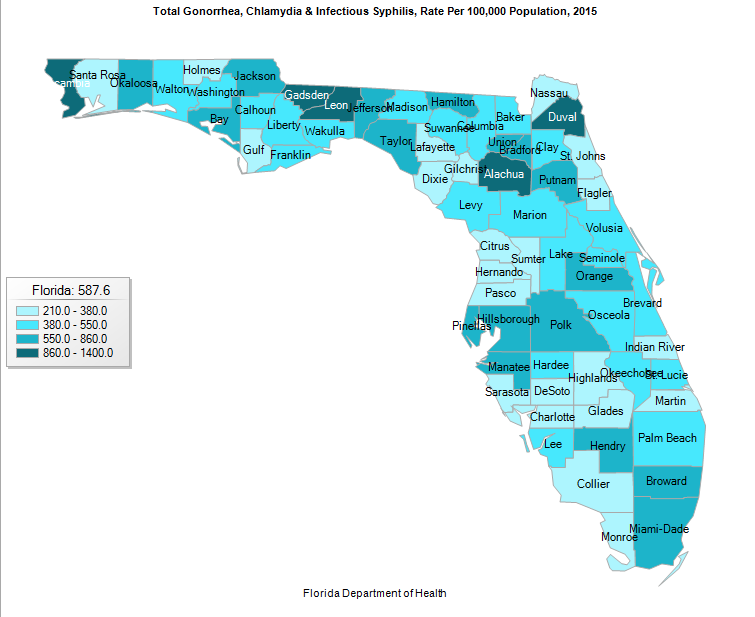
Except for a small dip between 2008 and 2009, total STD rates for this trio of diseases have been inching up in South Florida. Miami-Dade and Broward counties do not have the highest per capita rates for those diseases in Florida. That distinction belongs to Alachua, Leon, Escambia, Gadsden and Duval counties.
(But before you celebrate, consider this: Miami-Dade and Broward top the list for new HIV infection, with the former taking the number 1 spot and the latter falling into the second spot. The infection rate per capita for HIV in Miami was 47 per 100,000 while in Fort Lauderdale it was 41 per 100,000, according to the CDC. This was double those of other big cities including New York City and Los Angeles.)
The CDC figures are particularly troublesome because all three of the STDs can be cured with antibiotics, yet many cases go undiagnosed and untreated, which can lead to serious health issues including infertility, ectopic pregnancy, stillbirth in infants, and increased HIV risk. Because these STDs can be asymptomatic, the CDC recommends sexually active people under 25 get tested whether or not they experience symptoms.
In addition, public health officials are keeping an eye on gonorrhea cases. The disease is resistant to almost every antibiotic, and the only one that appears to work now is ceftriaxone. (Three years ago the CDC recommended a single ceftriaxone shot accompanied by an oral dose of azithromycin, and Prado says the dual therapy has been confirmed to work, without a resistance to ceftriaxone.)
People are having riskier sex
The increase in STD cases also come at a time when people report having less sex. One study published in the Archives of Sexual Behavior in 2017, for example, found that American adults, on average, had sex nine fewer times a year than they did in the late 1990s. Other data, from the General Social Survey, for example, reveals that the number of Americans reporting not having had sex in the past year increased from 18 percent to 22 percent over the past two decades. At the same time fewer young Americans 18 to 30 years old also say they are having sex twice a month or more,
But, as Prado points out, it’s not a matter of people having less sex but of people having riskier sex. “I think people are letting their guard down,” he explains.
In short, condom use is way down. Prado cites research that shows the use of condoms “decreasing steadily” in more than 15 years among adolescents, from 63 percent in 2005 to just under 54 percent in 2017. The downward trend is true for other demographics, including for both heterosexuals and gay and bisexual men.
He considers this an unintended consequence of improved treatment for HIV infections and a general lack of knowledge. In the past few years, drugs have transformed HIV from a death sentence to a treatable chronic disease. For some, condoms became optional. “But the [HIV} drugs don’t prevent STDs,” adds Prado.
Still, “I don’t think there’s one single reason we’re seeing this,” he says. “There are probably several factors to blame.”
Among them: dating apps and a cut in government funding for prevention and screening. “Technology, like the social dating apps, may contribute to individuals’ riskier sexual behavior,” Prado says.
Screening and treatment efforts are needed
On the other hand, public health officials have complained for years about the decrease in funding to state and local agencies. Federal monies are critical for both public and private organizations’ efforts in STD screening and treatment services, particularly for women but also for men.
“We need to do a lot more on that front [of prevention, education and screening] than we are currently doing, particularly with youth and with men having sex with men,” Prado says. “This is especially important among certain subgroups, Hispanics and other minorities, who are known not to have the same access to healthcare as non-Hispanic whites and who because of cultural stigma may not seek help [with their own doctors].”
Prado echoes CDC officials when he asks for a renewed commitment from health care providers to perform STD screening. “It should be part of the standard of care, just as we screen for other disease,” Prado says. “It’s the only way we might be able to reverse the trend.”
Tags: Dr. Guillermo Prado, sexual health, sexually transmitted infection, STD screening in Miami, STDs
