Sickle Cell Disease and Gene Therapy: A New Hope
An estimated 100,000 people in the United States live with sickle cell disease — a debilitating and life-threatening blood condition that predominantly affects people of African and Mediterranean descent, and Hispanic-Americans from Central and South America. For years, those who suffer from the disease have been treated with temporary solutions or with bone marrow transplantation from a donor, but new advances in gene therapy have opened doors to a possible cure using the patient’s own cells. Ofelia Alvarez, M.D., director of the Pediatric Sickle Cell Program at the University of Miami Miller School of Medicine, explains the potential breakthrough.
What is sickle cell disease?
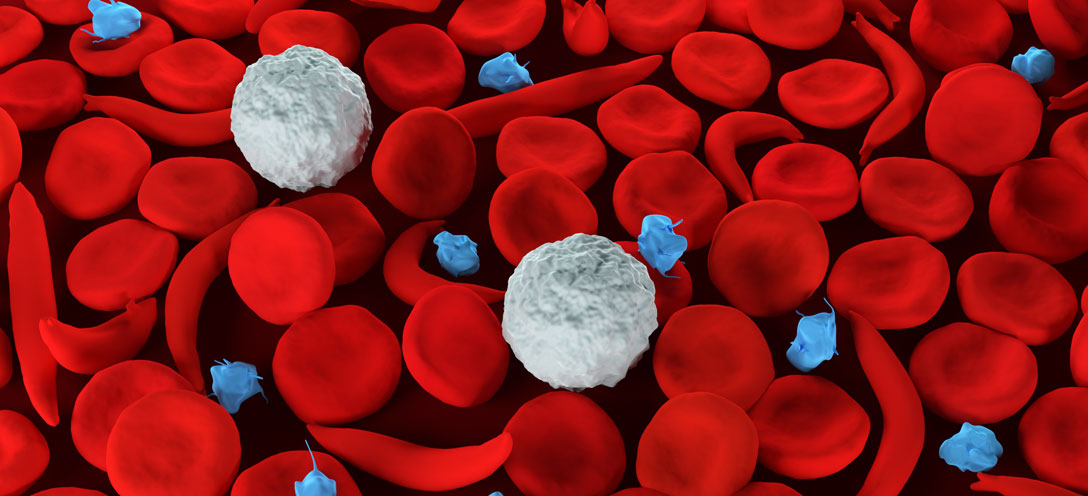
Sickle cell disease is an inherited chronic blood illness. It occurs when a person inherits the defective hemoglobin gene from each parent. “As part of newborn screening, all children in the U.S. and in many other countries are screened for sickle cell when they’re born,” Dr. Alvarez says.
Hemoglobin is the protein inside the red blood cells that carries oxygen in the body. Because of this gene mutation, the abnormal hemoglobin, called hemoglobin S, becomes unstable when it releases oxygen. Then the hemoglobin molecules begin to stack together to form many solid hemoglobin chains changing the shape of the red blood cell to a half-moon or sickled shape. Sickled red blood cells can stop blood flow to different parts of the body resulting in extreme pain or tissue damage. This condition also increases the risk of infection and stroke.
“This disease can lead to stroke because patients with sickle cell disease have vascular injury because of the sickling and the occlusion that they have in their body,” she says. “One of the areas that gets damaged is the blood vessels. Eventually, the blood vessels get very thick and the space inside them gets very small. This also happens in the brain. The arteries that are nourishing the brain thicken and then they get occluded. When you have an occlusion, then you have a stroke.”
How is it treated?
Pain Medicines: “Pain medications are very commonly used because pain is one of the most common complications of sickle cell disease,” Dr. Alvarez says. “Patients can take something mild, like ibuprofen, or they might need something as strong as morphine” administered in a hospital setting.
Disease-modifying therapy: The antimetabolite medication Hydroxyurea is “the most common disease- modifying therapy that we have,” she says. “It’s a mild chemotherapy pill that increases fetal hemoglobin. When babies are born, they have significant amount of fetal hemoglobin. Having a high fetal hemoglobin level is good because this interferes with the blood cell sickling process. As the child grows up, this level goes down. Increasing a patient’s fetal hemoglobin is the most effective way to modify this disease.”
Antibiotics: “What we call prophylactic antibiotics are administered for symptom and infection prevention in children,” Dr. Alvarez says. “Penicillin or erythromycin is given to children with sickle cell disease from about two months of age to about five years of age. Antibiotics are also given if patients have fever and are sick. The most common reason for antibiotic treatment is for the prevention of certain infections with encapsulated bacteria, such as pneumococcus, which is the most common bacteria and causes pneumonia and even life-threatening blood infection.”
Blood Transfusions: Blood transfusions can help get healthy red blood cells through donor blood and help prevent symptoms of sickle cell anemia.
“Blood transfusions can be administered acutely in the case of stroke, for instance, because stroke is one of the severe complications of sickle cell disease, and when patients have severe pneumonia or are very anemic,” Dr. Alvarez says. “Patients can also be put on chronic blood transfusions, which means they receive a blood transfusion every three to four weeks for stroke prevention.”
Bone Marrow Transplant: A bone marrow transplant can help the bone marrow make more normal, healthy red blood cells.
“We do this procedure at the University of Miami and Jackson Memorial Hospital, especially for children more than adults,” says Dr. Alvarez. “Patients with severe sickle cell disease who are intolerant to Hydroxyurea and have a match with a sibling or a parent are candidates for bone marrow transplant. Bone marrow transplant is considered to be a cure, as patients can go into remission after they’ve received one. Patients can get the blood-forming capacity of their bone marrow donor.”
What’s the latest research?
It’s called gene therapy.
This emerging treatment “is considered a transformative therapy,” Dr. Alvarez says, “meaning that the disease remains (is not cured). However, there is an increase in the fetal hemoglobin or the insertion of an anti-sickling hemoglobin that lowers the disease severity by the gene therapy product.” As a result, the patient no longer experiences sickle cell complications, such as pain. On December 8, 2023, the Food and Drug Administration approved two sickle cell gene therapy products. “These are really exciting times because we can offer these options,” she says.
With gene therapy, blood-forming stem cells are collected from the patient’s blood. This stem cell product is sent to a lab that genetically modifies the hemoglobin inside the red blood cells to alter the sickling process or make changes in the gene’s ability to make more fetal hemoglobin or add an anti-sickling hemoglobin, depending on the type of gene therapy chosen. The new, engineered product is infused back into the patient through a transplant after a brief chemotherapy treatment. Within weeks, the engineered stem cells begin producing new, healthier blood.
“In addition to being able to offer approved gene therapy products once they are fully on the market, we have a gene therapy study open at the University of Miami,” Dr. Alvarez says. “Clinical trials have already shown that gene therapy can increase fetal hemoglobin to levels of 40% or higher. Now, the question is, for how long and are there other side effects that we will see in the long run?” UM’s study will follow participants for 15 years to track the long-term success of this new therapy.
“It has the promise of really making a difference,” she says. “We want to be on the cutting edge of research, so I think we owe it to our patients to provide the newest therapies. We started screening patients for the gene therapy research protocol and making arrangements to start gene therapy with the commercial products for children with sickle cell disease starting at 12 years of age.”
In 2023, UM also received a 5-year grant from the U.S. Centers for Disease Control and Prevention to support state surveillance of individuals with sickle cell disease.
“We are one of 16 state awardees. We hope that knowing how many individuals have sickle cell disease in Florida could bring the opportunity to advocate for them and increase their care,” Dr. Alvarez says. “The goal is to change policy at the state level to benefit the individual. Most likely, we’re talking about 12,000 people affected by sickle cell disease in Florida.”
Updated in June 2024. Originally written by Amanda M. Perez for Inventum.
Originally published on: February 08, 2019
Tags: blood illness, Dr. Ofelia Alvarez, gene therapy, sickle cell disease
