What You Need to Know about Sinusitis
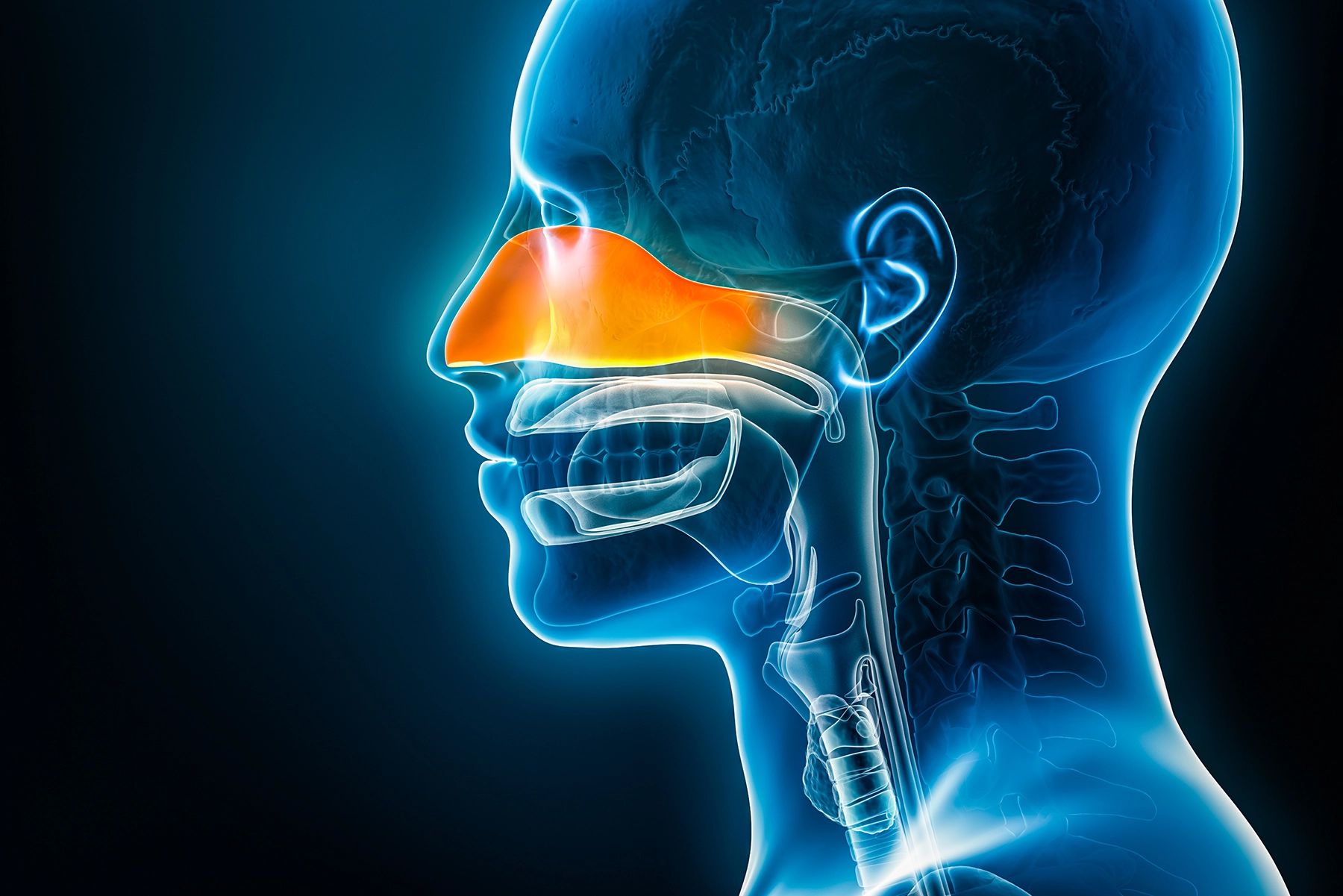
Most people don’t give their sinuses much thought — unless they cause problems. They are a critical part of your body’s defense system.
These air-containing spaces or cavities in the cheeks, nose and forehead are where mucus and germ-fighting immune factors are produced. An average of two pints of mucus flows per day over the surface of the nose, removing bacteria or mold and other harmful particles from the air you breathe like an air filter.
Due to infections, inflammation, or other factors, these spaces can occasionally become inflamed or produce too much mucus, generating symptoms of congestion or nasal blockage, pressure in the face, runny nose, postnasal drip, and/or loss of smell and taste. Many of these symptoms may be specific to viral infections such as a cold, flu or environmental allergies.
When sinusitis becomes chronic or long-lasting, it can lead to more severe complications if the inflammation isn’t treated.
The CDC reports that around 29 million Americans have chronic sinusitis.
Sinusitis versus cold or flu
Some of the confusion around sinusitis is that it seems pretty similar and can even appear alongside other common conditions, such as viral infections like a cold or flu or environmental allergies. Sinusitis (or inflammation of the sinuses) can be acute (symptoms lasting less than four weeks) or chronic (symptoms lasting more than three months). In acute sinusitis, a viral or bacterial infection is often the culprit. The symptoms of sinusitis are present along with other cold- or flu-like symptoms such as high fever, body aches, sore throat, runny nose, sneezing and more.
Symptoms of acute sinusitis generally resolve completely on their own if due to a viral infection or with antibiotics if a secondary bacterial infection is present. Examination of the patient’s nose after resolution reveals totally normal membranes without signs of inflammation. In chronic sinusitis, however, this inflammation is more permanent, with varying degrees of severity and permanent inflammatory changes of the mucosal membranes of the nose and sinuses on examination.
Roy R. Casiano, M.D., chief of the Rhinology and Endoscopic Surgery Division for the University of Miami Health System, says that chronic sinusitis is a unique medical condition distinctly different from a common cold, flu, or even allergies.
“Chronic sinusitis is not caused by an infection,” he says. “It’s an inflammatory disease that is more like other inflammatory diseases that affect other organ systems of the body, like rheumatoid arthritis or psoriasis, rather than an infectious disease like a cold or flu. The inflammation and congestion are caused by the overproduction of inflammatory factors produced by the body called cytokines in the sinuses.”
Certain subcategories of chronic sinusitis behave worse than others.
One factor that can compound the impact of chronic sinusitis is the presence of allergies.
Although allergies do not cause chronic sinusitis, the presence of two inflammatory conditions in the same patient exacerbates symptoms further and complicates their treatment. A 2021 review article in the journal Allergy, Asthma & Clinical Immunology reported that those with allergy symptoms were 3.1 times more likely to have sinusitis than those without allergy symptoms.
“If a person has both sinusitis and allergies, then both need to be controlled,” says Dr. Casiano. “Asthma can also be a contributing factor if a person has lower airway issues. In these cases, treatment for chronic sinusitis may require multiple specialists, including rhinologists, allergists and pulmonologists.”
By controlling both chronic sinusitis and allergies, asthma symptoms also tend to improve.
How to cope with chronic sinusitis
Acute sinusitis is frequently linked to infections like colds and flu and can be treated in a similar fashion. However, Dr. Casiano says chronic sinusitis often requires more drastic and ongoing lifelong treatment measures to manage the condition. If the condition is detected and treatment begins early, he says that it may be managed without surgery. This typically involves regular nasal irrigations and other therapies, such as nasal steroid sprays and oral antihistamines. Once prescribed or recommended by a doctor, these treatments can be done regularly at home to help clear the sinuses and keep symptoms from getting worse.
In many cases, however, Dr. Casiano says that chronic sinusitis is accompanied by the development of nasal polyps, or the formation of inflammatory “blisters” in the nose and sinuses that further contribute to the swelling and blockage that leads to other sinusitis symptoms.
An endoscopic surgical procedure, which is minimally invasive and performed on an outpatient basis, is often needed to remove those polyps or simply to open congested airways.
This procedure also helps facilitate long-term topical medical treatments that control inflammation by making the cavities more accessible to these treatments. By opening the sinuses, surgery makes the condition easier to treat moving forward and helps prevent complications like infections that can occur in inflamed sinuses or spread to other neighboring areas that share common walls with the sinuses, such as the brain or eye. Even after surgery, however, Dr. Casiano says that topical treatments are needed daily to wash away or dilute cytokines and keep chronic sinusitis symptoms from worsening.
Antibodies may help treat sinusitis
A relatively new class of drugs known as monoclonal antibodies have shown promise in treating several inflammatory diseases, including chronic sinusitis. For example, FDA-approved drugs like dupilumab (Dupixent) or mepolizumab (Nucala) have shown the ability to reduce stuffiness and even shrink nasal polyps in select patients with a specific subcategory of chronic sinusitis with polyps.
Even though chronic sinusitis cannot be cured, the disease can be managed with the right treatment regimen and regular consultations with your health care team.
In addition to following your doctor’s recommendations, steps such as avoiding allergens, not smoking, using a humidifier, and rinsing your nasal passages regularly at home can all help to reduce congestion.
Wyatt Myers is a regular contributor for UHealth’s news service.
Resources
1) Sinusitis, Johns Hopkins Medicine, 2024, https://www.hopkinsmedicine.org/health/conditions-and-diseases/sinusitis
2) Sinus Infection (Sinusitis), Cleveland Clinic, 2023, https://my.clevelandclinic.org/health/diseases/17701-sinusitis
3) Chronic Sinusitis, Mayo Clinic, 2023, https://www.mayoclinic.org/diseases-conditions/chronic-sinusitis/diagnosis-treatment/drc-20351667
4) Chronic Sinusitis, CDC, 2022, https://www.cdc.gov/nchs/fastats/sinuses.htm
5) Interview with Roy R. Casiano, M.D., chief of the Rhinology and Endoscopic Surgery Division for the University of Miami Health System.
6) The association between allergy and sinusitis: a cross-sectional study based on NHANES 2005–2006, Allergy, Asthma & Clinical Immunology, 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8710243/
7) Chronic Sinusitis, Cleveland Clinic, 2023, https://my.clevelandclinic.org/health/diseases/17700-chronic-sinusitis
Tags: antihistamines, Dr. Roy Casiano, nasal congestion, nasal passages
