Meet One of the Wonders of the Human Body: the Aortic Valve
Located between the left ventricle and the aorta, our largest artery, the aortic valve has three doors that open and close with each heartbeat to allow the blood to flow out and not return into the heart. Sometimes, though, the valve doesn’t function the way it should.
Diseases can affect the way the valve works. Aortic stenosis is the most common, affecting two percent of people 65 years and older. Another valve disease is aortic insufficiency or aortic regurgitation, when the valve becomes leaky, causing blood to flow back from the aorta into the left ventricle. In turn, this forces the cardiac muscle to work harder. People are also born with a bicuspid aortic valve, a genetic abnormality in which the valve has two leaflets or doors instead of three.
When the aortic valve isn’t working properly, surgery is the only cure and a life-saving option.
Left untreated, a diseased valve will affect heart function. For example, patients with aortic stenosis who don’t receive treatment have a 50 percent chance of death at five years and 90 percent at 10.
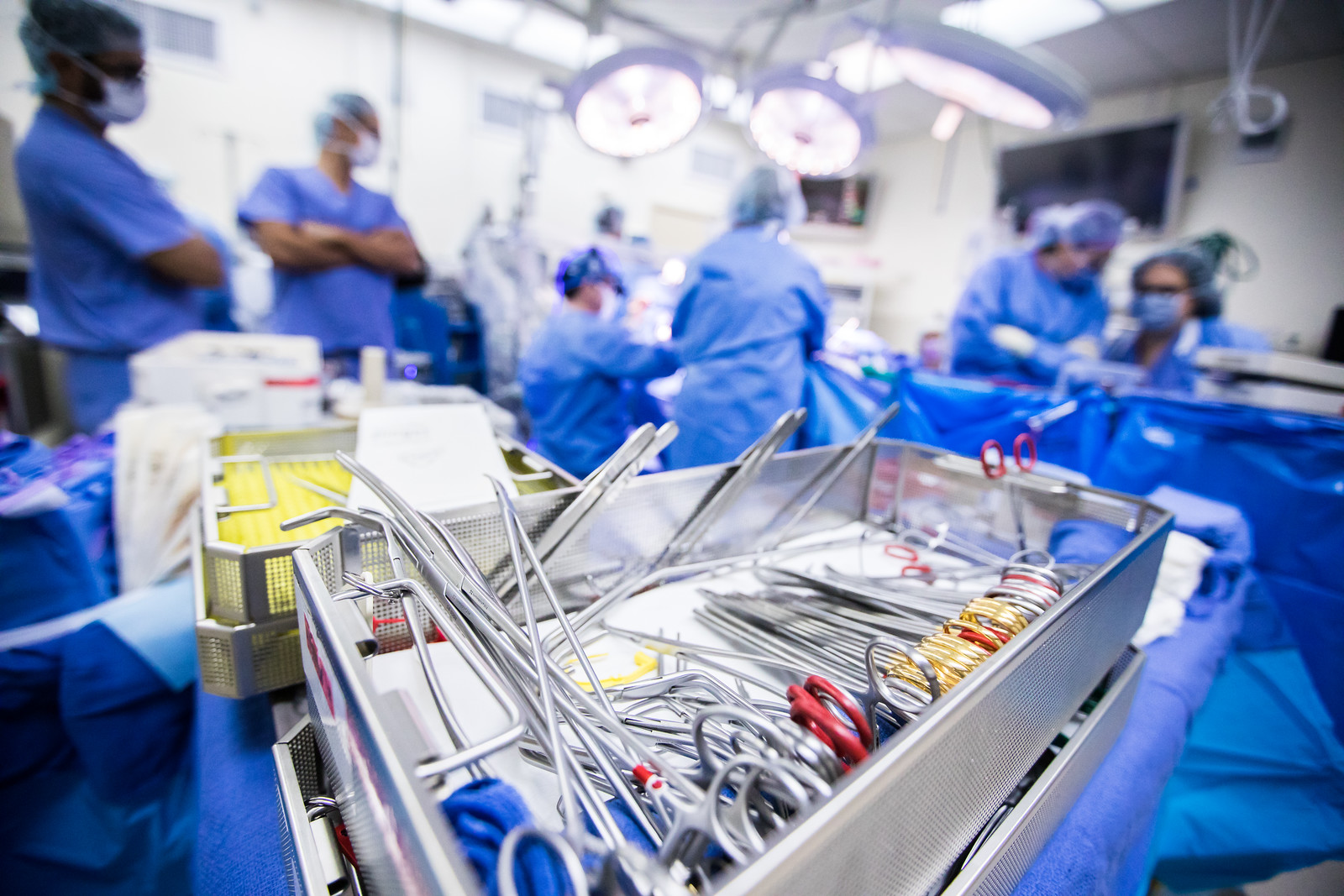
For years, aortic valve repair was limited to a heart surgery, which involved opening the chest, breaking the breast bone and operating while a machine did the pumping of the stopped heart. In the past few years, however, valve surgery has been undergoing a steady, if quiet, revolution, much of it led by pioneering Joseph Lamelas, M.D., who heads the cardiothoracic surgery team at the University of Miami Health System.
Less invasive aortic valve surgery
Starting in the early 2000s, Dr. Lamelas developed a series of minimally invasive techniques he dubbed the Miami Method. At a recent meeting of the American Association for Thoracic Surgery, an international association of cardiothoracic surgeons, Dr. Lamelas sat on a roundtable discussion of the future of aortic valve intervention. They discussed conventional minimally invasive techniques and a newer method.
“As we move forward, we’re going to see more and more patients seeking a less invasive approach,” Dr. Lamelas says.
And for good reason. Recovery from a traditional sternotomy can take months and the pain often lasts for weeks, as you would expect from a large incision along the chest. And though it has been a proven gold standard, with a good success rate, this approach has may not be the best option for high-risk patients, including those with prior cardiac surgery or those of advanced age. Minimally invasive surgery offers a safer option.
Dr. Lamelas’ minimally invasive techniques involve a 5 cm incision on the right side of the chest. Then, he uses special instruments to reach through the ribs to work on the valve. It has many benefits: a shorter hospital stay, shorter recovery time, less pain and better psychological reaction to the surgery.
TAVR: an option for high-risk cardiac patients
A relatively new approach is also offering another alternative, Dr. Lamelas adds. A procedure known as a transcatheter aortic valve replacement (TAVR) or transcatheter aortic valve implantation (TAVI) repairs the aortic valve by wedging a replacement valve into the disease valve’s place without removing it. As the new valve expands and takes over regulating blood flow, the old valve doors get pushed out of the way. (In the minimally invasive surgical procedure, surgeons replace the damaged valve completely.)
TAVI involves implanting the new valve by using a catheter that travels through a blood vessel — the femoral artery in the groin, through the aorta, and then within the existing valve.
Multiple trials have compared the use of TAVR in high-risk patients and found better results than traditional surgery, and this has been very encouraging.
Dr. Joseph Lamelas
As a result, TAVR has been adopted as a therapy of choice for extreme-risk patients. “TAVI offers patients who were previously inoperable a second chance.”
Newer randomized clinical trials have compared TAVI to sternotomy among medium and low-risk patients suffering from severe aortic stenosis. These found that the TAVI procedure was at least equivalent to traditional surgery, making TAVI a viable option across the patient-risk spectrum. Of course, like all medical procedures, TAVI is not without its risks. These include leakage around the valve, a higher risk of pacemaker implantation and us not knowing the durability of the TAVI valve.
Yet, Dr. Lamelas predicts more cardiac surgeons will move toward minimally invasive and transcatheter aortic valve replacement methods. “From a surgeon’s point of view, there’s going to be a growing need to embrace both,” he adds. “We have to be able to offer more options to the patient.”

Ana Veciana-Suarez, Guest Columnist
Ana is a regular contributor to the University of Miami Health System. She is a renowned journalist and author, who has worked at The Miami Herald, The Miami News, and The Palm Beach Post. Visit her website at anavecianasuarez.com or follow @AnaVeciana on Twitter.
Tags: aortic valve, cardiac surgery, Dr. Joseph Lamelas, heart surgery, Miami Method
