What’s the Best Nutrition Plan for Managing Diabetes?

Understanding what to eat and how much to eat can make or break your health when you’re living with diabetes. The most effective dietary recommendations for managing blood sugar spikes and maintaining a healthy weight have a few principles in common:
- less than 5 grams of added sugar per day
- less carbohydrates (45 grams max. per meal for women, 60 grams max. per meal for men)
- lots of fiber-rich vegetables
- relies on poultry, seafood, and lean meats (instead of fattier cuts)
- includes plant-based sources of protein
- limited full-fat dairy products
- avoids fried and processed foods
- minimal alcohol
- no sweetened, high-calorie beverages
How to balance your plate
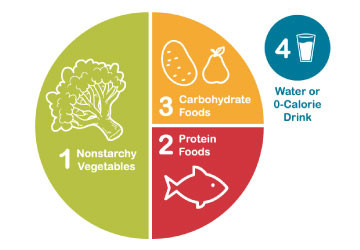
The American Diabetes Association (ADA) is the leading authority on diabetes research, tips and tools for those managing this condition. To simplify dining at home and restaurants, the ADA recommends the Diabetes Plate Method to create well-balanced, adequately portioned, satisfying meals to help manage your post-eating blood glucose levels. The best part is you can do this without counting calories or weighing your food.
The first step is to use a sensibly sized plate. A 9-inch dish or plate is enough to accommodate a full-sized meal. The bigger your plate, the more food you are likely to consume without even realizing it.
First, start with non-starchy vegetables (half of your plate).
The following veggies have fewer carbs and more fiber than their starchier counterparts. Fiber can help you feel full and satisfied. Don’t cheat yourself by filling half your plate with fried or sweetened vegetables.
- asparagus
- broccoli
- brussels sprouts
- cabbage (green, red, napa, bok choy)
- carrots
- cauliflower
- celery
- cucumber
- eggplant
- green beans, snow peas, sugar snap peas
- leafy greens (kale, collards, mustard, chard)
- mushrooms
- okra
- peppers (bell peppers, hot chilis)
- salad greens (lettuce, spinach, arugula, endive)
- squash (zucchini, yellow squash, chayote, spaghetti squash)
- tomatoes
Next, lean proteins should take up one-quarter of your plate.
Foods high in protein include both animal and plant-based products. You may be used to seeing half of your dinner plate filled with meat. But, when your goal is to manage your diabetes and your weight while protecting your heart from cardiovascular disease, you need a different dietary balance. Let non-starchy vegetables take center stage at every meal, and you’ll feel and see the difference.
Proteins from animal sources usually contain saturated fat, which may increase your risk of heart disease, heart attack and stroke. Lean proteins are lower in saturated fat and total fat. To avoid adding extra fat and calories, you can roast, bake, broil, boil, or air-fry lean proteins instead of deep frying or sautéing in butter.
Lean animal proteins include:
- chicken, turkey
- eggs
- salmon, cod, tuna, tilapia, swordfish
- shrimp, scallops, clams, mussels, lobster
- lean beef cuts (chuck, round, sirloin, flank, tenderloin)
- lean pork cuts (center loin chop, tenderloin)
- lean deli meats (turkey breast, chicken breast, lower-fat ham)
- cheese (reduced fat)
- cottage cheese (2% fat)
Plant-based sources of protein:
- beans (high in carbohydrates and fiber)
- lentils (high in carbohydrates and fiber)
- chickpeas, hummus (high in carbohydrates and fiber)
- nuts, unsweetened nut butter (high in fat)
- edamame
- tofu, which is made from soybeans
- tempeh
Fill the rest of your plate with carbs.
Carbohydrate foods have the biggest impact on blood sugar. You may assume that carbs are entirely off-limits when you’re managing diabetes. But, limiting your portion of carbs to 25% of your plate can help keep blood sugars from spiking too high after you eat. Plus, the types of carbohydrates you choose also make a difference.
Avoid highly refined carbs (like white bread, shelf-stable baked goods, and cereals) and added sugars (found in sodas, sports drinks, sweetened coffee beverages, candy, ice cream, pastries and some sauces and salad dressings). When reading food labels, pay attention not only to the carbohydrates but also the amount of added sugars.
You may be surprised that some heart-healthy foods are naturally higher in carbohydrates, even without any added sugars. These include starchy vegetables, beans, legumes, whole and dried fruits, and whole grains. These plant-based foods also provide dietary fiber that slows down digestion, fights hunger, improves bowel regularity and may help reduce blood sugar spikes.
Healthy carbs include:
- whole grains (brown rice, bulgur, oats/oatmeal, polenta, popcorn, quinoa)
- whole grain products (bread, pasta, tortillas) – whole grain flour is the main ingredient
- starchy veggies (acorn squash, butternut squash, green peas, parsnips, plantains, potato, pumpkin, sweet potato/yam)
- beans (black, kidney, pinto, navy, butter, garbanzo)
- whole fruits (fruit juices are stripped of valuable fiber) – keep portion size in mind, as some fruits are larger than a single serving
- unsweetened dried fruit
- dairy products (reduced-fat milk, unsweetened regular and Greek yogurt)
- plant-based, unsweetened milk (oat, soy, almond, flax)
What about fats?
People with diabetes can reduce blood sugar highs and slow down digestion (helping you stay fuller longer) by adding healthy fats to carbohydrate-rich meals and snacks.
Healthy fats include small portions of avocado, whole nuts, seeds (chia, hemp, sunflower), reduced-fat cheese or cottage cheese, unsweetened coconut flesh, and nut butters without any added sugars or oil.
Try adding more salads to your diet.
Salads don’t have to be boring side dishes. They can be surprisingly diverse with colorful starchy and non-starchy vegetables, lean proteins, beans or lentils, served warm, or topped with a small portion of cheese or chopped nuts or seeds for a satisfying crunch.
Skip the high-fat, sweetened bottled ranch dressing, and whip up your own creamy, tangy salad topper with olive oil, tahini, mustard, lemon juice, salt and pepper.
Diet is not the only factor you can control.
Finding the best diet to manage your diabetes is a process. It needs to address your body’s unique needs, lifestyle, and abilities. For example, what may work for someone in your family with the same condition may not work for you.
While food and portion changes can help, you may still need diabetes medication to support your health. Individuals with type 1 diabetes must continue to take insulin and other diabetes medications as prescribed, in addition to undergoing regular physician monitoring and bloodwork, to protect their overall health long-term. Those with type 2 diabetes can work to reduce their insulin and medication dependence with consistent dietary and lifestyle changes.
Additionally, everyone living with diabetes can support the effectiveness of their medication and diet while improving how they feel by committing to regular physical activity. Daily exercise will help you maintain a healthy weight, which reduces your risks for heart disease, heart attack and stroke. The ADA guidelines recommend a minimum of 150 minutes of weekly physical activity.
Dana Kantrowitz is a contributing writer for UHealth’s news service.
Medically reviewed by the following University of Miami Health System providers:
Natalie M. Sinel-Rojas, M.S., R.D., L.D.N., CPhT, diabetes educator
Aleida Saenz, APRN, FNP-BC, CDCES, diabetes educator
Maddison Saalinger, M.S., R.D., L.D.N., C.D.C.E.S., diabetes educator
Tags: blood sugar levels, Diabetes care in Miami, diet for diabetics, endocrinology, food tips for blood sugar, nutrition care in Miami