Convalescent Plasma: A Promising COVID-19 Treatment
As the world eagerly awaits a vaccine for COVID-19, researchers are looking into existing therapies that might help treat the novel coronavirus, particularly for patients who suffer the most severe symptoms. Among them is Maria Luisa Alcaide, M.D., director of the Infectious Diseases Research Unit at the University of Miami Health System.
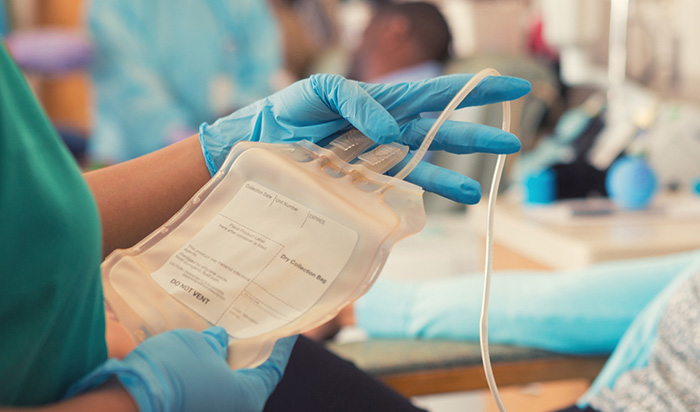
Along with Shweta Anjan, M.D., assistant professor of clinical medicine, the two physician-scientists have launched a new initiative to use convalescent plasma as therapy for stricken patients. The multi-site national project, “Use of Convalescent Plasma for Severe COVID-19,” has been approved by the U.S. Food and Drug Administration’s Expanded Access Program, which allows doctors’ use of investigational drugs or devices outside of clinical trials in the case of patients with life-threatening illnesses.
“This is for severely ill COVID patients, those who are in ICU,” explains Dr. Alcaide. “It’s been used before and it’s been successful, so we have a lot of hope for it.”
Actually, convalescent plasma transfusions have been around for more than a century. It was a go-to treatment for the Spanish Flu of 1918 and also more recently for patients who have contracted Ebola, SARS and H1N1 flu. In the era of COVID-19, researchers believe it could be used more extensively, particularly since there are no specific anti-viral therapies for this new disease.
At the time of this writing, Drs. Alcaide and Anjan have treated four patients. Though it’s “too early to assess the long-term benefits,” the team is optimistic and hoping to move forward with more infusions.
Here’s the rationale behind this treatment:
Plasma, which is light yellow, is the liquid part of blood and it accounts for 55% of it. (Platelets and red and white blood cells account for the rest.) Plasma contains antibodies, or immunoglobulins, those hard-charging body soldiers that fight bacteria, viruses and other pathogens. Antibodies hang out in plasma for a while, ready to strike if the invader returns. They’re also highly specialized, which means they protect a person only for the specific invader they’ve already fought.
Borrowing antibodies through plasma is called passive immunity. It’s particularly helpful when no treatment or vaccine exists. Active immunity, on the other hand, is when your body produces its own antibodies, or you get the antibodies through a vaccine.
Doctors like Dr. Alcaide are now using plasma collected from patients who have already recovered from COVID-19. If the past is any indication, they know that these “borrowed” antibodies will help a patient fight off the disease. Think of it as a reinforcement platoon.
“The idea is that if given to a patient who is struggling to fight off [the infection], it will help them in that. This is for people who haven’t been able to fight it on their own.”
DR. ALCAIDE
She adds that there’s no clear data on the best time for the infusion, but thinks the optimal schedule would be before a patient develops breathing problems. “We think it may be best before they’re intubated and begin to decompensate,” she says, adding that going on a mechanical ventilator can lead to complications in a patient.
Currently Drs. Alcaide and Anjan have infused patients with a single dose equal to 200 to 300 ml of plasma. At this time, there are no plans to add a second infusion. Side effects are similar to a blood transfusion. “You can have inflammatory responses, like a mild allergic reaction, but these are uncommon.”
Anyone who has had COVID-19 can donate their plasma
But, they can’t do so until 28 days after testing positive for the virus or after having repeat negative results from a swab specimen. They have to be 18 years of age or older. Already several notable people have publicly announced they will be donating their plasma, including Miami Mayor Francis Xavier and actor Tom Hanks. Dr. Alcaide says she hopes this will encourage others to do the same.
“One of the limitations we face is the availability,” she says. “As time goes on and more people are diagnosed, we’ll need more.”
UHealth has partnered with OneBlood to collect and publicize the need for plasma. The donation is actually quite simple, Dr. Alcaide adds. A phlebotomist draws blood, which then goes through a machine that separates the plasma out. This plasma is kept and stored by the blood bank, while the remaining blood (minus the plasma) is returned to your body. You can donate more than once.
“I hope that people who tested positive will consider donating,” Dr. Alcaide says. “While this is still an experimental treatment, we do have data that show it’s very promising.”

Ana Veciana-Suarez, Guest Columnist
Ana is a regular contributor to the University of Miami Health System. She is a renowned journalist and author, who has worked at The Miami Herald, The Miami News, and The Palm Beach Post. Visit her website at anavecianasuarez.com or follow @AnaVeciana on Twitter.
Tags: COVID-19, M.D, Maria Luisa Alcaide, Shweta Anjan
