Osteoporosis and Osteopenia: What’s the Difference?
By some accounts, about 54 million Americans have osteoporosis, or low bone density, which can lead to bone fractures.
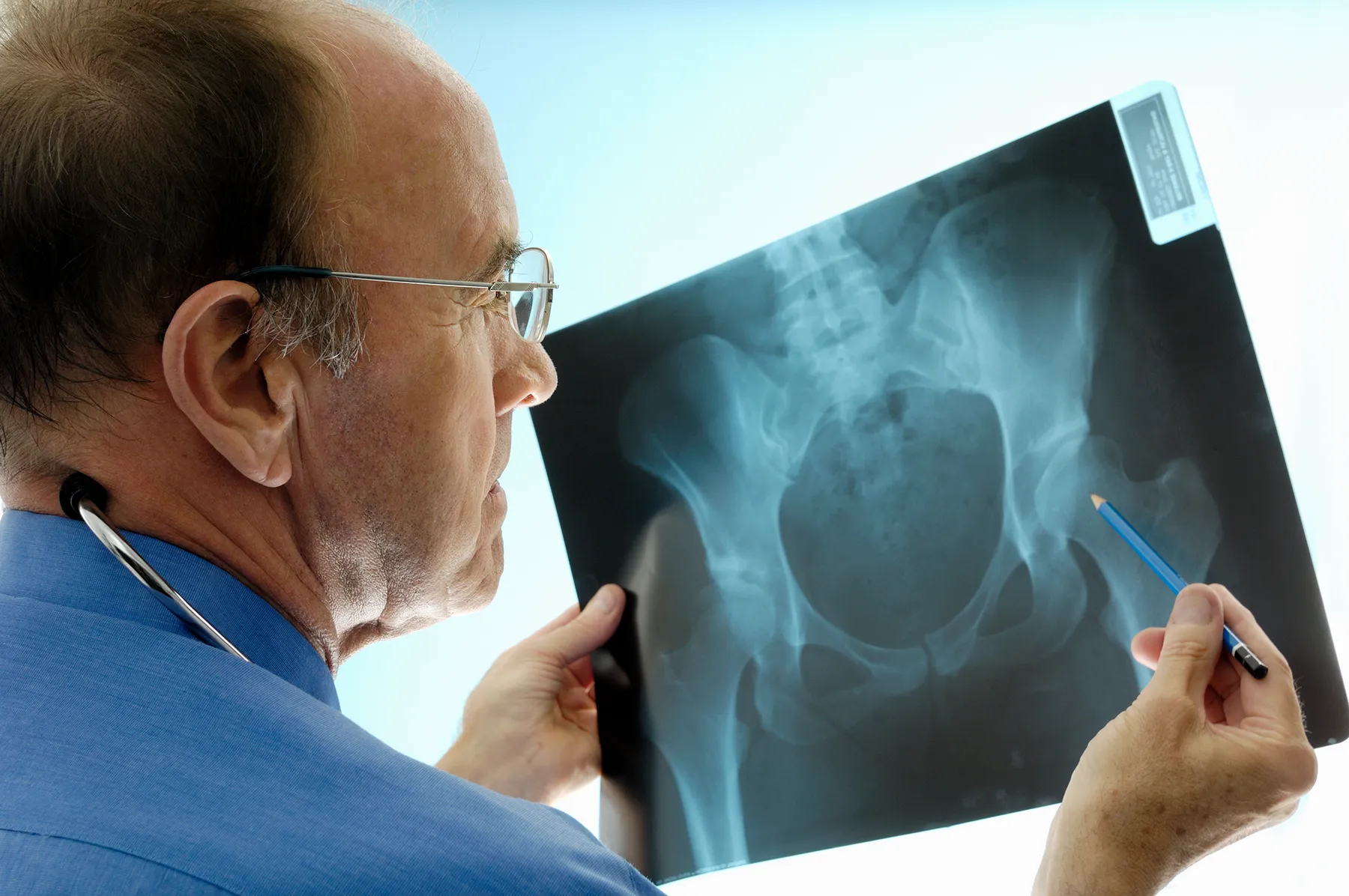
Bone mineral density (BMD) is the measurement of how much bone mineral is in your bones. Your BMD estimates the chances of breaking a bone from a normal activity or a simple, non-traumatic fall. The problem is with knowing you have low BMD.
Osteoporosis is a silent disease with no symptoms—until you break something
Knowing where you stand with bone mineral density and other risk factors really ups your chances for avoiding fractures and all the problems associated with them.
Let’s start with measuring bone mineral density.
The National Osteoporosis Foundation recommends you have a central DXA (dual energy x-ray absorptiometry) test of the hip and spine for:
- Women age 65 or older or women of menopausal age with risk factors
- Men age 70 or older or men age 50-69 with risk factors
- Anyone who:
- Has broken a bone after age 50
- Has had an X-ray of your spine showing a break or bone loss in your spine
- Has had a height loss of ½ inch or more within one year or a total height loss of 1½ inches from your original height
Talk to your doctor to see if you are a candidate for bone mineral density testing and to help you determine your risk.
Osteopenia means actual bone loss.
Aging is the most common risk factor for osteopenia. After your bone mass peaks, your body breaks down old bone faster than it builds new bone. That means you lose some bone density every year. You may have osteopenia if your bone density measurement is at least one standard deviation below the average bone density of 25-year-olds. If you are 50 or older and slimly built, you will not have a 25-year old’s bone density.
Women lose bone more quickly after menopause. If you lose too much, your bone mass may drop low enough to be considered osteopenia, or low bone density. About half of Americans older than age 50 get osteopenia.
Many people think that having osteopenia but not osteoporosis is nothing to worry about.
“I disagree. There are so many people with osteopenia. Because of the sheer numbers, there are more fragility fractures in that group than in the group with osteoporosis. But it is not just your bone density measurement that determines your risk for fracture. Other factors figure in. You need to talk to your primary care physician or an endocrinologist to look at the whole picture,” says Dr. Silvina Levis, an endocrinologist and expert in osteoporosis with the University of Miami Health System.
One of the most common fracture risk assessment tools for people age 50 and older is called FRAX (Fracture Risk Assessment Tool).
Each indicator impacts your fracture risk:
- Bone mass loss increases with age.
- Women are at a higher risk for osteoporosis and related fractures, but men can also develop osteoporosis.
- This is one condition where having low weight increases your risk.
- Your height-to-weight ratio can help determine how frail you are or whether you are too overweight.
- Do you have a previous fracture? Your FRAX score will be higher if you’ve had a fracture that occurred without known trauma or if you’ve broken a bone caused by trauma that would not usually cause a fracture in a healthy person.
- Or has a parent ever fractured his or her hip? If your mother or father had a hip fracture, your risk is higher.
- Do you smoke? Smoking is a controllable risk factor for osteoporosis and weaker bones.
- Are you taking steroid medications? Whether used to treat allergies, autoimmune conditions, and other health problems, they can also interfere with the formation of new bone tissue and with your absorption of calcium.
- Do you have rheumatoid arthritis? This autoimmune condition is associated with a higher risk of osteoporosis.
- Any conditions that can cause secondary osteoporosis? This includes conditions such as type 1 and type 2 diabetes, hyperthyroidism, chronic liver disease, premature menopause (prior to age 45), and several other conditions.
- Do you drink three or more alcoholic drinks of any kind per day? Excessive alcohol consumption raises the risk of osteoporosis.
- What is your bone mineral density (BMD)? On the questionnaire, if entering your BMD, you must select the brand of the scanner used to measure your bone density, or you can enter your T-score.
Your FRAX score will be calculated based on your answers and give you a 10-year risk percentage of a major osteoporotic fracture and a 10-year risk percentage of a hip fracture. A FRAX score of more than 3 percent for a hip fracture or more than 20 percent for a major osteoporotic fracture means you should consider treatment along with lifestyle changes. A lower FRAX score may also require treatment, depending on other clinical factors.
Dr. Levis also likes the Australian fracture risk calculator called GARVAN, because it also includes in the risk picture the number of falls you have had in the last year.
“If you fall frequently, your risk for fracture increases.”
She says that even if you have osteopenia and not osteoporosis, based on bone density scores, other risk factors could make it a good idea to start treatment to prevent fractures before osteoporosis sets in. That’s why having this discussion with your doctor is so important. For more information on osteoporosis and BMD testing, visit the National Osteoporosis Foundation website.
Mary Jo Blackwood, RN, MPH, is a contributing writer for UMiami Health News. Based in St. Louis, MO, and Colorado, she has written medical articles and webpages for consumer publications and major university health centers.
Tags: Dr. Silvina Levis, DXA, Fracture Risk Assessment Tool, FRAX score, GARVAN score, osteopenia, osteoporosis
